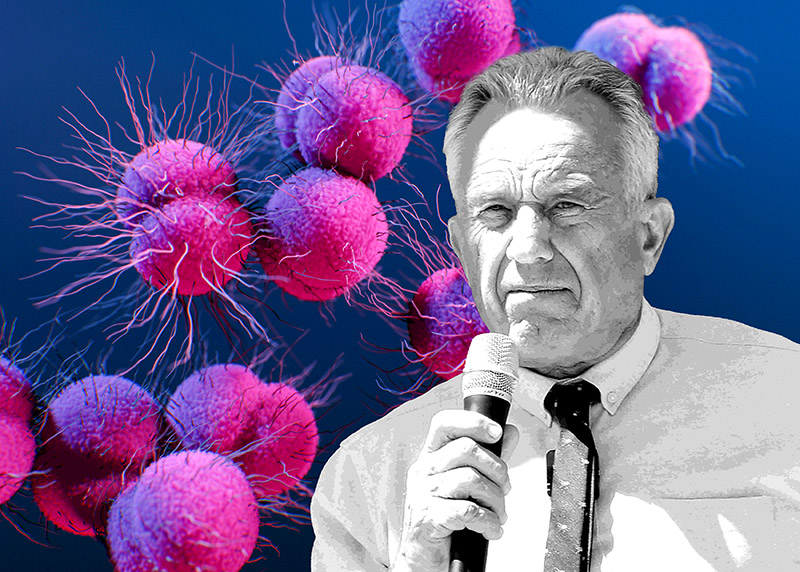
California becomes first state to require insurance to cover at-home STI tests
Bill seeks to connect partners of those who test positive for STIs with treatment, and requires syphilis screenings for those who are pregnant.

Insurance companies in California will now be required to cover the costs of at-home test kits for sexually-transmitted infections, including HIV, syphilis, and chlamydia.
Under a bill that went into effect earlier this month — the first of its kind in the nation — not only will insurance be required to cover the cost of the at-home tests, but the number of health care providers that can offer STI tests will be increased, and providers will be required to provide “expedited partner therapy,” or prescribe antibiotics or treatments to the sexual partners of those who test positive for STIs.
The bill, authored by State Sen. Richard Pan (D-Sacramento), a pediatrician, and co-authored by State Sen. Scott Wiener (D-San Francisco), was signed into law by Gov. Gavin Newsom (D) in October.
Pan said the bill was intended to help curb infection rates in California, which have increased over the past few years, by expanding access to testing and treatment options.
According to statistics from the California Department of Public Health, the number of syphilis, chlamydia, and gonorrhea infections in California — taken together — rose more than 62% from 2013 to 2019.
In addition, COVID-19-related lockdowns and social distancing, as well as the shuffling of some medical staff to prioritize treating COVID-19-related illnesses, have made it more difficult for state residents to seek out free or low-cost STI testing, especially in rural areas where testing locations or services may not be as readily accessible.
The bill also requires expectant parents to be screened for syphilis during the first and third trimesters of pregnancy in order to protect infants from contracting congenital syphilis, rates of which rose 232% in California from 2015 to 2019, according to the Centers for Disease Control and Prevention. More than 8% of congenital syphilis cases in the state resulted in stillbirths in 2019, reports HIV Plus Magazine.
Advocates of the law say at-home tests offer privacy options for those concerned about visiting an STI clinic or speaking with health care providers about sexual issues, and make it easier for those in rural areas where medical care is not as easily accessible, to test themselves.
Californians with private insurance can take advantage of the coverage immediately, but out-of-pocket costs — if anything — will depend on the type of plan they have, whether their provider is in-network, or if they fall into a category that makes them eligible for free screening, reports Kaiser Health News.
But those on Medi-Cal, California’s Medicaid program, may have to wait for coverage to take effect due as the program updates its billing practices, meaning providers may be reticent to order tests until those issues are resolved.
That said, most health care advocates see the bill s a positive step toward combating the rise in infections.
In a statement issued in October when the bill was signed into law, a coalition of community health and advocacy groups — APLA Health, Black Women for Wellness Action Project, Essential Access Health, Fresno Barrios Unidos, the Los Angeles LGBT Center, and the San Francisco AIDS Foundation — praised the bill as essential to curbing STI rates.
“For the past six years, STI rates have reached record highs in California,” the statement read. “Rising STI rates have gone largely ignored for far too long. STI prevention is an equity issue. Pre-existing structural barriers to STI treatment and care have only worsened during the COVID-19 pandemic, disproportionately impacting Black, Indigenous and people of color, rural regions, California youth, and LGBTQ+ communities.”
They continued: “SB 306 is the bold action California needs to turn the tide on rising STI rates. The bill seeks to expand the tools and resources that health providers can use to increase access, reduce STI transmission and improve health outcomes across the state in partnership with advocates, local organizations and community members.”
Advocates hope that other jurisdictions will soon follow suit by requiring insurance to cover the costs of tests. Currently, Alabama and the District of Columbia will send free STI kits to residents who request them, but neither jurisdiction requires insurance coverage for them.
The National Coalition of STD Directors is sending free kits to people through health departments in Philadelphia, Iowa, Virginia, Indiana, Puerto Rico, and Navajo County, Arizona. “I Want the Kit,” a project of Johns Hopkins University, also offers free STI testing kits to residents of Maryland and Alaska.
Support Metro Weekly’s Journalism
These are challenging times for news organizations. And yet it’s crucial we stay active and provide vital resources and information to both our local readers and the world. So won’t you please take a moment and consider supporting Metro Weekly with a membership? For as little as $5 a month, you can help ensure Metro Weekly magazine and MetroWeekly.com remain free, viable resources as we provide the best, most diverse, culturally-resonant LGBTQ coverage in both the D.C. region and around the world. Memberships come with exclusive perks and discounts, your own personal digital delivery of each week’s magazine (and an archive), access to our Member's Lounge when it launches this fall, and exclusive members-only items like Metro Weekly Membership Mugs and Tote Bags! Check out all our membership levels here and please join us today!




















You must be logged in to post a comment.